The Common Perception
- The use of narcotics in healthcare settings leads to increased instances of addiction. A high percentage of people who are prescribed narcotics for pain control will continue to use them even after their pain has been resolved, due to other pleasurable effects.
- Nurses are hesitant to administer narcotics when prescribed due to the perceived risk
- Clients’ fear of potential addiction can lead to refusal of narcotic use, even when it is the most effective option
- Clients’ families perceive the use of narcotics as a reflection of the client’s weakness or dependence
- The use of narcotics in healthcare settings leads to increased instances of addiction. A high percentage of people who are prescribed narcotics for pain control will continue to use them even after their pain has been resolved, due to other pleasurable effects.
In 2012, 5.2% of those using opioids for pain in Canada reported they abused them. (Centre for Mental Health and Addictions, n.d.)

Misconceptions vs. Reality
“It is a common misunderstanding, even among some health professionals, that the therapeutic use of scheduled drugs creates large numbers of addicted clients. In fact, prescription drugs rarely cause addiction when used according to accepted medical protocols. Nurses should administer these medications as prescribed for the relief of client symptoms without undue fear of producing dependency (Adams, M.P., et al, 2018).”
All people will get addicted if they use narcotics for long enough.
Reality: most patients do NOT get addicted. Addiction is an uncontrollable urge to get high. This is often linked to environmental factors (Centre for Mental Health and Addictions, p. 3). The body will develop a need for it over time. This is a physical dependence, not addiction.
It is easy to overdose on narcotics.
Reality: if you follow your doctor’s orders, there is a very low chance of having an overdose. Taking alcohol and other sedative-type drugs with your opioid prescription will increase the risk of an overdose, but otherwise, long term use of opioids are safe. (DeGroote, n.d.)
Addiction is a choice.
Reality: while the first decision to use may be a decision, the resulting addiction is not due to lack of character or the person being too “weak” to stop. Often there are a lot of contributing factors such as trauma, environment, mental health issues, to name a few. (Centre for Mental Health and Addictions, p. 3)
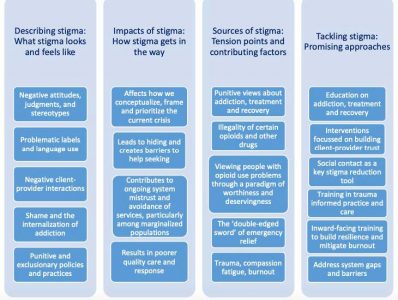
What is stigma? Where does it come from?
What can we do about it?
“We still see addiction as being a choice or just this bad thing and . . . why should I be paying for your lifestyle choices that you’re making? . . . But the reality is that, every day, people are in hospitals getting treated for lifestyle-related [things], right? —you know, we don’t shame people who have diabetes because you ate too much ice cream or too much sugar. We don’t shame people who have cancer because of smoking. We just treat them.”
-Anonymous
What happens when you stop taking narcotics?
Abrupt withdrawal will induce physical withdrawal symptoms, which for opioids tend to be flu-like, such as nausea, chills, and/or diarrhea. Gradually tapering off the opioids will lower the chance of withdrawal symptoms.
Adams, M.P., Urban, C.Q., El-Hussein, M., Osuji, J., King,S. (2018). Pharmacology for Nurses: A pathophysiological approach, pp 290.Pearson Canada: Toronto, ON. Centre for Mental Health and Addictions. (n.d.). Opioids and Addiction: A primer for Journalists. Retrieved from Centre for Mental Health and Addictions: http://www.camh.ca/-/media/files/5217-opdsaddic_primer-pdf.pdf DeGroote, M. J. (n.d.). Canadian Guidelines for Safe and Effective Use of Opioids for Chronic Non-Cancer Pain. Retrieved from National Pain Centre: http://nationalpaincentre.mcmaster.ca/opioid/cgop_b_app_b04.html MentalHealth Commission of Canada, 2019. Stigma and the Opioid Crisis: Final Report. Retrieved from https://www.mentalhealthcommission.ca/sites/default/files/2019-07/Opioid_Report_july_2019_eng.pdf?fbclid=IwAR1hXKT2ktOoROPzQha3vDjlZp-MrX5909HwMMYRSvagu2KGio5wvX9yALY Photo: Jenna Miller, 2019.

